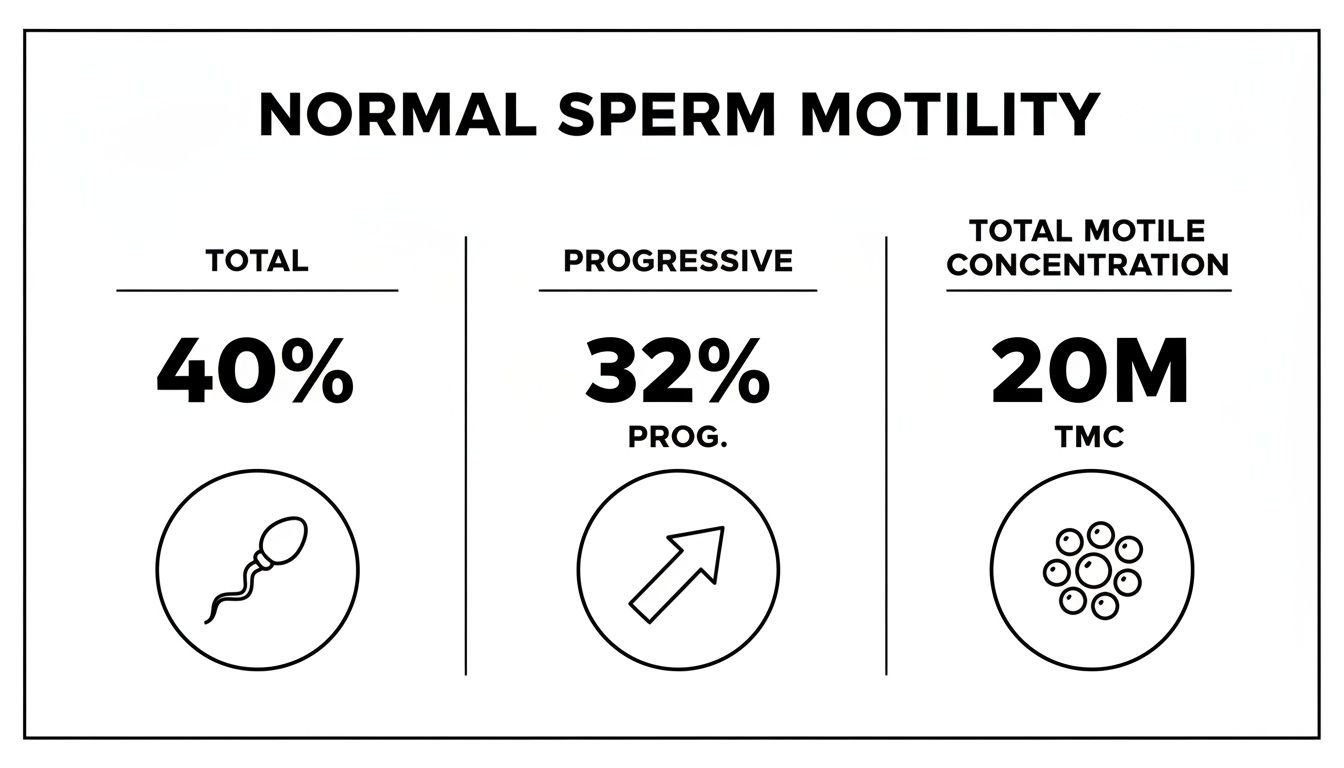
Normal Sperm Motility means that 40% or more of sperm are moving overall and at least 32% are swimming forward, with a Total Motile Count above 20 million. This snapshot gives a clear, immediate sense of male fertility health. Comparing these numbers to a semen analysis result helps men understand where they stand.
Many men just want a straightforward benchmark before diving into detailed fertility data. Following World Health Organization reference ranges, experts agree these figures offer a reliable gauge for natural conception odds.
Key Figures For Normal Sperm Motility
It’s one thing to read percentages—it's another to know what they mean in real life. These key figures set expectations for both men and their healthcare providers.
Normal Sperm Motility Ranges
Below is a quick reference table to visualize what each threshold means in practice.
Normal Sperm Motility Ranges
| Measure | Threshold | Clinical Implication |
|---|---|---|
| Total Motility | ≥40% | Enough moving sperm to navigate toward fertilization site |
| Progressive Motility | ≥32% | Forward swimmers capable of fertilization |
| Total Motile Count | ≥20 million | Boosts odds for natural conception |
This table gives men and clinicians a shared language for discussing test results.
Healthy motility is as crucial as sperm count for successful natural conception.
Men who meet or surpass these benchmarks generally show stronger movement profiles and enjoy higher fertilization chances.
- Offers an immediate go/no-go indicator for further testing
- Serves as a foundation for targeted motility improvement plans
Understanding Sperm Motility Basics

Sperm motility isn’t a random toss-up—it’s a performance score showing how effectively sperm cells navigate the male reproductive tract in their journey toward fertilization. Picture each sperm as a miniature motorboat, its flagellum acting like a propeller powering a straight or curved path.
Simply counting sperm doesn’t tell the whole story. Movement matters most.
Key Motility Types
- Total Motility: The percentage of sperm showing any motion, even if it’s in tight circles.
- Progressive Motility: The percentage of sperm cruising forward in mostly straight lines or wide arcs.
While total motility casts a wide net—including both sprinters and slowpokes—progressive motility zeroes in on the true sprinters: the cells most likely to reach the destination first.
“Healthy motility is like lining up sprinters on a track—only the fastest contenders make it to the end.”
Cohort studies have reported average motility around 60–65%, with plenty of individual variation. To account for that spread, clinicians lean on reference thresholds rather than strict averages. These motility thresholds underpin the WHO reference values of ≥40% total motility and ≥32% progressive motility.
Visualizing Sperm Movement
Under the microscope, progressive sperm stream ahead like boats cutting a canal, while non-progressives loop or spin, burning energy without moving forward.
- Tracking software times straight-course swimmers—much like timing cars on a racetrack.
- Total motility simply counts every vessel in motion, no matter the direction.
In practice, slides are warmed to 37°C to recreate body conditions. Technicians then use high-powered microscopes or computer-assisted analysis software to map each cell’s path. Based on speed and trajectory, cells are classified as progressive or non-progressive and tallied accordingly.
High motility signals well-fueled engines firing at peak efficiency. Low motility suggests swimmers that tire before covering the distance.
These fundamentals set the scene for a full semen analysis, where motility metrics become part of your comprehensive fertility picture.
Next Steps With Hera Fertility
- Order a physician-signed lab requisition online in minutes—no clinic visit required.
- Select from 250+ CLIA-certified labs across the USA and Canada for sample collection.
- Get an AI-powered Hera SmartScore that translates complex motility data into clear, actionable insights.
- Discuss your results with our fertility experts and chart your personalized plan.
Stop guessing and start understanding your sperm motility. Hera Fertility is here to guide you.
How Semen Analysis Measures Motility
A semen analysis goes beyond a simple headcount. It shows how sperm actually swim under a microscope or through computer-assisted systems.
Technicians often compare each sperm to a tiny car on a busy highway—speed, direction and traffic flow all matter.
Tracking motility is like monitoring traffic flow: you want to know how fast cars are going, where they’re headed, and if they’re stuck.
Lab Steps For Measuring Motility
Preparing the sample starts with a gentle mix and a brief rest. Then slides are warmed to 37°C, mimicking the body’s natural temperature and keeping sperm alert.
From there, two methods unfold:
- Manual tracking with a microscope and stopwatch
- Computer-assisted tracking using video capture software
Cells that push themselves forward earn the label progressive motility, while those that spin in place or make tight loops are non-progressive.
| Classification | Description |
|---|---|
| Progressive Sperm | Moves forward in straight lines or wide arcs |
| Non Progressive Sperm | Moves but fails to swim straight or stay on track |
This breakdown turns speed and direction into clear categories.
Combining Motility With Count And Volume
Motility is just one piece of the puzzle. Labs also measure volume and concentration, then blend these figures into a single metric.
For instance, a 3.0 mL ejaculate at 50 million/mL with 40% motility equals a Total Motile Count of 60 million, a number often seen as favorable for treatments not requiring specialized lab procedures. Discover more about TMC calculation in our full guide at Healthcare Utah.
Want to dive deeper? Check out our guide on how to read semen analysis results.
Interpreting Combined Metrics
Looking at motility alone can be misleading. It’s like knowing traffic speed without counting how many cars are on the road.
By focusing on Total Motile Count, you get a snapshot of real-world swimming strength. This single figure becomes a roadmap for next steps, whether that’s lifestyle tweaks or a specialist consult.
Visualizing Motility Under The Microscope
At the bench, technicians look for subtle quirks in movement. They watch for head vibrations and the rhythm of the tail whip.

- Tail whip speed measures propulsion power
- Straight-line velocity tracks forward travel
- Pattern coherence checks group behavior
Microscopic movement patterns unlock a deeper view of male fertility health.
These insights turn raw data into practical advice. Now, you have the full picture to guide your next move.
Clinical Significance Of Abnormal Motility
When sperm motility dips below 40% total or 32% progressive, we start to look for deeper clues. Think of motility as horsepower in an engine: less power means a tougher journey.
Reduced movement may reflect lifestyle choices or medical conditions slowing down those tiny swimmers. Early detection here can guide timely intervention.
Common Causes Of Low Motility
- Smoking exposes sperm to toxins and can slash motility by up to 30% over time.
- A diet low in antioxidants leaves sperm with less fuel, resulting in sluggish swimmers.
- Prostate infections can damage the flagella, hindering forward progress.
- Repeated heat exposure—from hot tubs or tight underwear—raises testicular temperature and slows movement.
- A varicocele (enlarged veins in the scrotum) acts like traffic congestion, stalling sperm propulsion.
Case in point: John watched his progressive motility drop from 45% to 25% after years of chain smoking.
A man with 20% progressive motility often has roughly half the natural conception odds compared to men at 32% or higher.
When progressive motility falls below 20%, natural pregnancy rates can plummet without support.
Tipping Points For Intervention
| Progressive Motility | Relative Pregnancy Odds |
|---|---|
| ≥32% | Baseline 100% |
| ~20% | ~50% |
| <10% | <25% |
Actions To Protect Motility
- Quit Smoking to cut out harmful toxins.
- Boost Your Diet with fruits, nuts, and omega-3s for antioxidant support.
- Keep Testicles Cool by avoiding extended heat (saunas, laptops).
- See a Urologist if you experience scrotal discomfort.
These steps often lead to noticeable gains. However, motility is only one piece of the puzzle.
Volume and count feed into the Total Motile Count, painting a fuller fertility picture. If motility stays low after lifestyle tweaks, further evaluation is critical.
Check out our guide on asthenozoospermia and low motility in our article on asthenozoospermia and low motility.
Next steps may include targeted lab tests, a scrotal ultrasound, or hormone panels to pinpoint root causes.
A specialist can determine if varicocele repair or antibiotic therapy is needed.
Hera Fertility simplifies this process. Order a semen analysis, get AI-powered results with clear motility insights, and receive expert guidance on improving movement.
Understanding these clinical thresholds empowers men to act early and boost their chances of conception.
Strategies To Improve Sperm Motility

Making a few targeted tweaks in your routine can lift sperm motility in just a few months. From what’s on your plate to how you wind down before bed, each choice counts toward stronger swimmers.
Dietary Adjustments
- Add antioxidants such as vitamin C, vitamin E, and CoQ10 to protect sperm from oxidative stress.
- Incorporate omega-3 rich foods like salmon, walnuts, and chia seeds to support healthy cell membranes.
- Stock up on colorful fruits and vegetables for a natural spectrum of vitamins and minerals.
When John swapped soda for a daily glass of orange juice, he saw his motility climb by 15% after three months.
“Loading up on antioxidants is like upgrading from regular to premium fuel,” says a seasoned male fertility coach.
Exercise And Circulation
- Aim for 30 minutes of brisk walking or cycling five days a week to boost blood flow.
- Add light strength sessions twice weekly; it can help maintain healthy testosterone levels.
- Skip post-workout saunas or long hot baths to keep testicular temperature in check.
In just eight weeks, David’s shift from evening hot tubs to jogs pushed his progressive motility from 28% to 36%.
| Loose Underwear | Benefit |
|---|---|
| Loose Underwear | Keeps testes cooler |
| Hydration | Maintains optimal semen |
| Supplements | Targets specific nutrient gaps |
Stress Management And Sleep
Chronic tension can drag down sperm quality, while solid rest restores hormonal balance.
- Carve out 10 minutes for deep breathing or meditation each morning.
- Stick to a regular bedtime to secure 7–9 hours of sleep nightly.
- Power down screens at least an hour before bed to promote natural melatonin.
Loren upped his water intake to 2.5 liters daily and noticed a silkier semen texture on his follow-up test.
Temperature Control And Clothing
Small habits matter here, too:
- Switch briefs for boxers at night.
- Avoid placing laptops directly on your lap.
- Use cooling packs if you work in a warm environment.
Next Steps For Men
- Craft a simple daily plan combining these diet, exercise, and sleep tips.
- Schedule a follow-up semen analysis to track your progress.
- Check out our guide on improving sperm health with proven strategies: https://herafertility.co/improve-sperm-health
Start with small changes and let consistency deliver results.
When To Seek Professional Help
If motility stays below normal benchmarks after three to six months of targeted lifestyle tweaks, it’s time to see a specialist. You might assume eating better and exercising will rev up those slow swimmers, but persistent low motility often needs medical insight.
Keep an eye out for warning signs—testicular discomfort, unexpected fatigue or subtle hormonal shifts. These clues, paired with poor motility, can point to issues like varicocele (enlarged veins in the scrotum) or hormonal imbalances. Jotting down symptoms in a simple log helps your doctor connect the dots.
- Persistent Low Motility: below 40% total or 32% progressive after months
- Testicular Pain or Swelling: discomfort that doesn’t resolve or worsens
- Hormonal Symptoms: low libido, energy dips, mood shifts
What To Expect At Your Consultation
During your first appointment, your specialist will review your semen analysis alongside your health history. Blood tests and a hormonal panel—checking testosterone, thyroid and more—reveal hidden imbalances. You may also undergo an advanced semen analysis to see how motility responds under different conditions.
For men in their late 30s or 40s, age adds urgency since sperm quality naturally declines. If your timeline is tight, faster intervention makes sense. Going in prepared with targeted questions ensures you leave with a clear, actionable plan.
“A specialist visit turns confusion into clarity by matching your motility data with targeted tests for real answers.”
Key Questions To Ask Your Expert
- Which testicular or hormonal exams do you recommend first?
- How do my motility results compare to standard reference ranges?
- What timeline should I expect for seeing improvements after treatments?
Mapping out a follow-up plan gives you focus and peace of mind. When self-help stops moving the needle, professional care bridges the gap. Hera Fertility supports you through every step—from testing to ongoing guidance—so you never face male fertility challenges alone.
Next Steps With Hera Fertility
- Upload your existing lab reports for a free AI analysis
- Schedule a specialist appointment
- Prepare questions about your sperm motility and overall fertility health right now
Frequently Asked Questions
Many men wonder what normal sperm motility looks like and, more importantly, how to act on that information. It’s perfectly normal to have questions about testing schedules, the impact of health events, and best practices for improving motility.
Testing Frequency
How often should you check sperm motility in a semen analysis? Experts typically recommend repeating tests every 3 to 6 months. That window aligns with the full sperm production cycle, giving you meaningful trend data rather than a single snapshot.
- Schedule each analysis after 48 to 72 hours of abstinence for a consistent baseline.
- Avoid testing immediately after a fever or illness to prevent misleading results.
Can illness or fever affect sperm movement? Absolutely. An elevated body temperature can slow swimmers for up to three months.
Illness can reduce motility by as much as 20% until recovery is complete.
Lifestyle Improvement
Will lifestyle changes improve sperm motility naturally? In many cases, yes. Simple shifts in diet, exercise, and stress management often translate into measurable gains.
Start by adding antioxidants like vitamin C, vitamin E, and CoQ10 to your daily routine. Pair that with moderate, regular exercise to boost circulation—just be sure not to overheat the testes.
- Practice deep breathing or meditation to lower cortisol levels.
- Opt for loose-fitting underwear to keep the testicles cool.
Abstinence Period and Accuracy
Why does the abstinence period matter for motility results? Too short a break may undercount swimmers, while too long can dampen motility. Aim for 48–72 hours to capture the most accurate snapshot of your sperm’s performance.
Regularly discussing your results with a healthcare provider ensures you stay on track. Use Hera Fertility’s AI-driven insights to turn motility data into clear, personalized action steps.
Track your progress with follow-up tests and adjust habits as you go. Monitor key metrics like progressive motility and share them with your doctor.
Stay proactive about your fertility journey—and reach out when you’re ready to take the next step.